There are numerous vulvar skin disorders – some are not so serious, other are rather serious. Vulvar skin disorders usually arise from infections or irritations caused by cleaning agent or other hygiene or grooming activities such as shaving and waxing.
As the name implies, vulvar skin disorders affect the vulva.
The vulva is the outer part of the vagina, the female reproductive organ that accepts the penis during sexual intercourse. The vulva is made up of the labia majora and the labia minora, the inner and outer fleshy covering of the vagina.
Vulvar skin disorders are the conditions that cause irritation, itching, pain, or burning sensation to the labia majora and minora of the vagina and surrounding skin. While some of the disorders are mild and will go away with time, others need professional care and medication before they leave.
From reading this article, you will be able to recognize some vulvar skin disorders, their causes and prevention. In case they have started already, how they can be treated. Some of the vulvar skin disorders that abound include folliculitis, vulvodynia, Bartholin gland cysts, contact dermatitis and many more. For this article, we will focus on folliculitis and contact dermatitis.
Vulvar Skin Disorders
-
Folliculitis
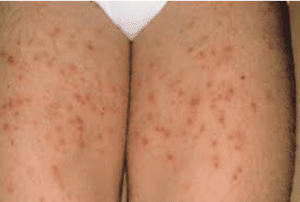
Folliculitis is a skin condition in which the hair follicles – hole or point from which hair grows – become inflamed due to shaving or waxing. It is usually not a serious condition as it happens almost every time some people shave. If you have shaved and noticed some bumps on your shaved area, that is folliculitis.
However, it becomes a serious condition when the bumps become infected by the bacteria, staphylococcus. It might cause the inflamed area to swell, become red, and have pus in it. It is worse if these bumps become itchy.
Causes of Folliculitis
Folliculitis is caused by bacteria (staphylococcus and pseudomonas), fungi, and sometimes, viruses.
Types of Folliculitis
There are two types of folliculitis and they are:
- Superficial Folliculitis
This type of folliculitis occurs when only part of the hair follicle is affected. It is also further divided into different forms, depending on its cause of infection.
-
Bacterial Folliculitis
This form of superficial folliculitis is common. It is caused by the infection of an inflamed skin area by staphylococcus bacteria. It is characterized by itchy, pus-filled bump.

Staph bacteria are almost always on the skin and only cause problem when they are introduced into the body.
-
Razor Bumps
This is a common occurrence with men that have curly hairs as they have to shave very close to the skin in order to remove ingrown hairs. This damages the skin and causes dark bumps that later become scars.
It also happens with people who shave or wax their genital areas.
-
Hot tub Folliculitis
The appearance of this form of superficial folliculitis is round and red. It is usually itchy and is caused through infection by pseudomonas bacteria. This bacterium is found in many places, including hot tubs and pools that have poorly regulated pH and chlorine levels.
-
Pityrosporum Folliculitis
This form is caused by yeast infection. It is usually invasive, red, and itchy. It is commonly found around the neck, chest, face, upper arms, shoulders, and back.
- Deep Folliculitis
Deep folliculitis occurs when there is a complete infection of the hair follicle. Its forms include:
-
Sycosis barbae
-
Boils and Carbuncles
This occurs when the staph bacteria on your skin get into your body through cuts – which can be caused around your vagina and other places during shaves – and completely infect the hair follicle.
-
Gram-negative folliculitis
This occurs when you’re undergoing treatment for acne, using antibiotics.
-
Eosiniophilic folliculitis
This occurs in people with weakened immunity due to infectious diseases such as HIV. It causes serious itching and recurring patches of bumps. It usually leaves dark spots after healing.
Self-Care Tips for Folliculitis
Sometimes, folliculitis goes away without treatment. However, it usually happens that way when you take extra care of yourself with these tips you can use at home.
-
Regularly Clean the Affected Parts
Clean the affected parts of your skin twice daily with antibacterial soaps. Make sure you’re gentle while at it and avoid sharing your cleaning items with anyone. When you remove clothes from your body, wash the ones that have touched the affected skin immediately.
-
Apply soothing lotions
Using lotions that have soothing properties help you reduce the itchiness of the affected skin area. They are available over-the-counter and mostly contain hydrocortisone.
-
Use warm, moist washcloths as compress
Insert washcloths in warm water, preferably containing salt at a ratio of 1 tablespoon of salt to 2 cups of water, and press it against the affected skin area. Do this several time daily to help rid the area of moisture and relieve discomfort.
-
Over-the-counter Antibiotics work
Antibiotics that are available over-the-counter can be of benefit. They are available in creams, gels, and washes.
-
Guard your skin
It might be wise to stop shaving. It (barber’s itch) usually clear some weeks after shaving.
Treatment of Folliculitis
The treatment of folliculitis depends on the causative agent as any of viruses, fungi, or bacteria could cause the infection. It usually involves medication, surgery, or laser treatment.
It is important to note that infection may reoccur after treatment. If this happens, another round of treatment is advised, except otherwise decided by your doctor.
Medication
Folliculitis treatment through medication is achieved through creams, pills, and soaps or washes.
Bacterial folliculitis is usually tackled with antibiotic creams, gels, or washes. However, in severe cases, antibiotic pills are prescribed by doctors, to be used orally.
For folliculitis caused by fungus, antifungal creams, pills, and washes are recommended. While for not-so-serious eosinophilic folliculitis, steroid creams that help to improve the itching symptom is usually prescribed by doctors.
Other treatment options are minor surgery – where minor cut is made on your boil to extract the pus; and Laser hair removal treatment.
-
Contact Dermatitis
Contact dermatitis is a condition that is characterized by itching – which can be mild or severe, red rash on the affected area of the skin, and sometimes, bumps or blisters. It is usually a reaction to an irritant that has come in contact with the skin.
Usually, around the vagina, the cause of contact dermatitis could be shampoos or bleach and detergents used to wash underpants.
Prevention of Contact Dermatitis
-
Avoid Irritants
Do not wash your underpants with detergents and bleaches that contain irritants. Avoidance of these irritants that may cause contact dermatitis when they touch your vaginal skin will help you avoid vulvar skin disorder as well.
-
Moisturize often
Applying moisturizer to your skin regularly helps to strengthen your skin against these irritants. They do not have as much effect as they will on a weaker skin.
Treatment and Self-Care
To treat contact dermatitis, you will be advised to stop the use of the irritant, which is also a self-care tip for contact dermatitis, a vulvar skin disorder.
For treatment, use of oral medications are prescribe in extreme cases. The medications usually contain antihistamine, corticosteroid, or antibiotics to combat itching, inflammation, or bacterial infection respectively.
Topical creams, another treatment option also contain these itching, bacteria fighting, and inflammation reduction properties. However, it is used for milder cases of contact dermatitis.
Conclusion
Vulvar skin disorders are conditions that cause the skin around the vagina to be itchy, red, swollen, or crust. This might happen due to irritation from a substance used around the vagina and vulva or a cut infected by a microorganism. There are different types of skin disorders and this is because they can be caused by different agents even though they present similar symptoms.
Vulvar skin disorders can be treated using creams, gels, and in extreme cases, pills. These treatment options aim at reducing inflammation, itchiness, and infection.
Recurring vulvar skin disorders can happen. When they do, contact your doctor.
Related reading
- 10 Self – Care Tips To Deal With Vaginal Odour
- 10 Tips to Boost Vaginal Birth Recovery
- Vaginal Thrush Treatment, Symptoms, and Causes
- Appropriate Sore Throat medication for Pregnant Women
- Menorrhagia (Heavy Menstrual Bleeding): Causes, Treatment, and Self-Care
- Bacterial Vaginosis: Causes, Diagnosis, and Treatment
- Vaginal Thrush: Home Treatment and Self-Care
- What You Need to Know About In Vitro Fertilization (IVF) Process
