Mastitis denotes inflammation within the breast, typically stemming from an infection. This condition commonly occurs in women during breastfeeding, particularly within the initial 6-12 weeks postpartum. It’s important to note that experiencing mastitis does not increase the likelihood of developing breast cancer.
What are the symptoms of mastitis?
Women afflicted with mastitis may experience various discomforts and symptoms indicative of feeling unwell, such as fatigue and body aches resembling flu-like symptoms. Additional signs may encompass:
- Pain in the breast
- Swelling of the breast
- Presence of a tender, red, wedge-shaped region on the breast
- Elevated temperature or a breast that feels warm or hot to the touch
- Sensation of burning while breastfeeding
- Discharge from the nipple
- Fever
- Chills
- Nausea or vomiting
It’s noteworthy that mastitis typically affects one breast at a time.
What causes mastitis?
Mastitis commonly originates from germs, typically bacteria present on the skin or in the baby’s mouth. These bacteria gain entry into the breast through openings in milk ducts or cracks in the nipple.
Infection becomes more probable when milk becomes trapped within the breast. The accumulation of stagnant milk fosters bacterial growth, leading to infection. Milk can become trapped due to inexperienced or improper breastfeeding techniques. Additionally, blockage of a milk duct can result in milk backing up within the breast.
Factors that may increase the risk of developing mastitis include:
- Having sore or cracked nipples
- Employing only one breastfeeding position (utilizing various positions helps ensure complete drainage of the breast)
- Wearing tight-fitting bras or applying pressure to the breasts, which can impede milk flow.
Read Also: Turmeric While Breastfeeding: Benefits, and Tips
How is mastitis diagnosed?
During your medical consultation, your doctor will inquire about your symptoms and conduct a thorough examination of the affected breast. They will assess for signs of swelling, tenderness, and the presence of a painful, wedge-shaped area on the breast, which is indicative of mastitis.
If you are not breastfeeding and exhibit symptoms suggestive of mastitis, your doctor may recommend additional diagnostic tests. These tests may encompass a breast ultrasound, MRI (magnetic resonance imaging), mammogram, or biopsy to further investigate the condition.
Can mastitis be prevented or avoided?
Here are some fundamental breastfeeding techniques aimed at reducing the likelihood of developing mastitis:
- Ensure your baby latches onto the nipple with their mouth wide open.
- Allow your baby to fully empty one breast before transitioning to the other breast.
- Vary your baby’s position during feedings to ensure all areas of the breast are effectively drained.
- Use your finger to break the suction if you need to interrupt a feeding.
- Avoid wearing tight-fitting bras or breast pads that may keep your nipples moist after breastfeeding.
- Whenever feasible, expose your nipples to air.
- Inform your doctor or lactation consultant if you experience nipple pain during nursing.
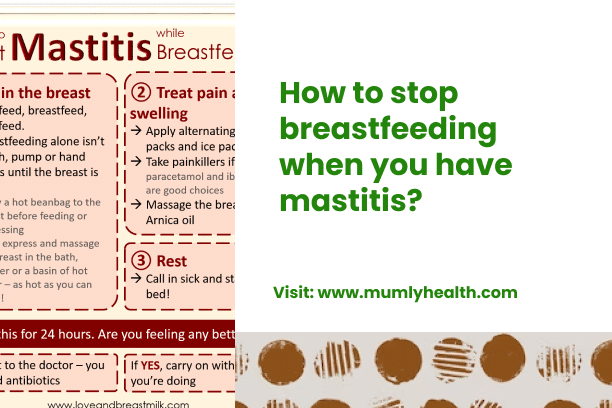
Mastitis treatment
In cases where breast infections occur, sometimes they resolve without intervention. If you detect symptoms of mastitis, consider the following steps:
- Breastfeed on the affected side every 2 hours or more frequently to maintain milk flow and prevent excessive milk accumulation.
- Massage the area gently, starting from behind where it feels sore and using a circular motion towards the nipple.
- Apply warm, moist compresses to the sore area to alleviate discomfort.
- Wear a supportive, well-fitting bra that isn’t overly tight to avoid constriction of milk ducts.
If you don’t notice improvement within 24 hours of implementing these measures or if your symptoms worsen, contact your doctor. They may prescribe medication, typically antibiotics, to address the infection. It’s crucial to complete the entire course of antibiotics to prevent antibiotic resistance.
Over-the-counter pain relievers like acetaminophen (Tylenol) or ibuprofen (Advil) can help alleviate pain, and warm showers may also offer relief.
Despite discomfort, it’s important to continue breastfeeding during mastitis. Your breast milk remains safe for your baby, though some infants may notice a change in taste. Ceasing breastfeeding could exacerbate the infection by allowing germs to proliferate in remaining milk. If nursing isn’t possible, pump your breasts to remove milk.
Adequate rest and increased fluid intake can expedite recovery. If symptoms worsen, consult your doctor promptly.